General Guidelines // Precautions
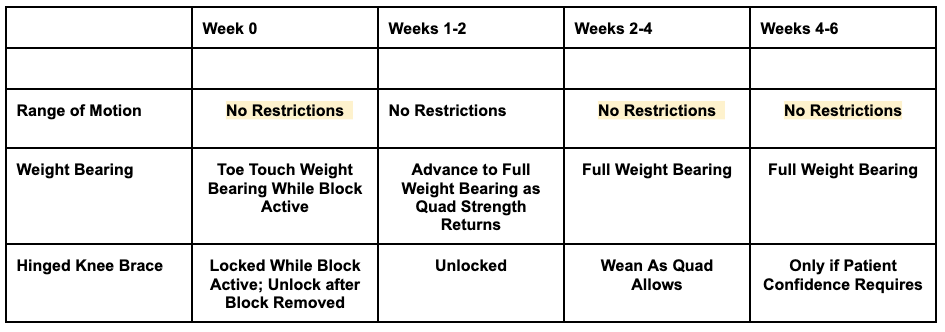
-Wear brace / immobilizer at all times except during bathing and physical therapy for the first 2 weeks. Keep brace locked in extension while the block is active. The brace can be unlocked after one week and worn until quad strength normalizes.
-Keep incisions clean & dry for the first two weeks. Incisions will be examined at the 2-week visit.
-Edema / Effusion management & attaining full extension are the two top priorities immediately after surgery.
-Bilateral crutches should be used for ambulation for 1-2 weeks and criteria must be met before discontinuing the crutches.
-Track or treadmill running should not be started before 4 months post-op
-This protocol, as well as most, is a general guideline. Patients should not be progressed to the next phase until they demonstrate proper form with all activities and functional criteria are met in the current phase.
-Properly assess the whole body and incorporate treatment for loss of mobility and stability throughout.
-There is concern regarding strain values on ACL graft with open chain activities in the first 6 weeks of healing, limit open chain activities in the first 6 weeks to light- load, short-arc quadriceps exercises
-Exercises listed are suggested for each phase and not comprehensive. Feel free to add exercises that fit the goals and precautions. Since not all patients have the same equipment, exercises must be individual tailored by a patient’s attending physical therapist.
-Blood Flow Restriction (BFR) has compelling evidence that it can improve the return of quadriceps size and strength when used postoperatively with low-intensity resistance training (LIRT) after ACL reconstruction. However, not everyone will have access to BFR. Additions to the protocol involving BFR are in Red and are optional as circumstances allow.
-Reducing post-operative swelling is the most important initial objective after surgery. Increasing blood circulation at a time where patients are not fully weight bearing expedites the resolution of postoperative swelling and also decreases the chances of a blood clot. The Geko is a battery powered, disposable neuromuscular electrostimulation device which can be worn at the knee to gently stimulate the common peroneal nerve. This stimulation activates the calf and foot muscle to increase blood flow and reduce postoperative swelling. The increase in blood flow is equal to 60% of normal walking at a time when patients are not normally walking. The Geko is an optional addition to help reduce swelling and decrease the risk of a blood clot after surgery. Additions to the protocol involving Geko are in Green.
PRE-OPERATIVE PHASE
Goals:
- -Diminish inflammation, swelling, knee effusion, and pain
- -Restore normal ROM (especially knee extension)
- -Restore voluntary muscle activation
- -Protect the knee from further injury (If no meniscus injury is present, crutches and a brace are not needed as long as activity is limited from running/cutting/pivoting)
- -Educate on goals, expectation, and precautions
Exercises/Treatments:
- -AAROM/PROM knee flexion (Goal Range of Motion Before Surgery 0 Degrees of Extension and 120 degrees of Flexion)
- -Passive knee extension
- -Bike or seated stepper
- -Isometric quadriceps setting
- -Straight leg raises
- -Gentle CKC exercises: mini squats, lunges, step-ups
- -Gait training
- -Cryotherapy and muscle stimulation as needed
- -Compression wrap as needed for swelling
IMMEDIATE POST- OPERATIVE PHASE (days 1 to 7)
Goals:
- -Diminish joint swelling and pain
- -Restore full passive knee extension
- -Restore patellar mobility and prevent adhesions
- -Re-establish quadriceps control
- -Gradually improve knee flexion
- -Normalize gait pattern with assistive device.
Precautions:
- -Brace / immobilizer applied to knee, locked in full extension and worn at all times when ambulating and up from a recumbent position.
- -Weight Bearing — two crutches, WBAT
Suggested But Not Comprehensive Exercises/Treatment (Day 1)
- -Ankle pumps
- -Overpressure into full, passive knee extension
- -Quad sets with muscle stimulation
- -Gastroc towel stretch
- -GameReady/Ice for 20 minutes every hour if needed.
- -Weight shifts while in brace
- -PROM 0-90 degrees
Exercises/Treatment (Day 4 to 7)
- -Continue all previous exercises / treatment
- -Multi-angle isometrics at 90 and 600
- -Knee extension 90-400
- -Mini squats and weight shifts
- -Proprioception and balance activities (i.e. cone walking / step overs)
- -PWB with crutches (NWB if Major Bone Bruise or Meniscus Repair) – Full Passive extension 1st PT visit (0 deg only, no hyperextension)
- -Long Sitting Ext Hang, Prone Hangs prn
- -Begin immediate Patellar Mobilizations Grade I, II all directions
- -Cryotherapy / Compression prn – QS w/ Russian ES &/or Biofeedback
- -SLR w/Assist prn for lift off -> Progress to Independent SLR by 7 days
- -SLR Abd, Add, Ext Independent.
- -HS isometrics – at 60-90 deg Flexion
- -Ankle Pumps Independent – HS, calf stretching
MODERATE PROTECTION PHASE (Week 2-4)
- -Criteria for Phase Progression:
- -Minimal joint effusion
- -Full passive knee extension
- -Good patella mobility
- -Quad control (ability to do SLR w/ no extension lag)
- -PROM 0-90
- -Proper ambulation with assistive device
Goals
- -Wean from Crutches
- -Maintain symmetrical knee extension / hyperextension
- -Gradually increase knee flexion
- -Diminish swelling and pain
- -Normalize patella mobility
- -Improve muscle control and activation
- -Restore proprioceptive / neuromuscular control
- -Wean from Brace as Quad and Patient Comfort Allow
Exercises /Treatment (day 8-21)
- -Continue all relevant previous treatment
- -Progress LE flexibility (hamstring, calf, hip mobility)
- -Eccentric quadriceps strengthening (40-1000)- Squats, Standing hamstring curls
- -Seated Stepper or Stationary Upright Bicycle (1150 required for bicycle)
- -Progress proprioception drills
- -PWB – focus on good Gait mechanics (heel – toe)
- -Maintain Full Passive Extension – (progress towards hyperextension if present)
- -Passive Flexion to 105 deg. – Independent SLR w/ progressive weights as tolerated
- -Standing Weight Shifts (For isolated ACL only)
- -Continue Patellar Mobs (Gr 2-3)
- -Continue Cryotherapy prn for effusion control
- -Independent QS if able to maintain 3+/5 or greater muscle tone
- -Ankle Manual Resistance program – (DF, INV, EV)
- -HS prone/standing curls as allowed by AROM
- -Begin Aquatic Therapy walking gait training (for isolated ACL pt’s)
- -Begin Proprioceptive training in water (for isolated ACL pt’s) – Calf raises – 2 leg
PROGRESSIVE STRENGTHENING, NEUROMUSCULAR CONTROL PHASE (week 4-12)
Criteria for Phase Progression:
- -Active ROM 0-1200
- -Minimal to no full joint effusion
- -Minimal / no joint line or patellofemoral pain
- -Weaned from Brace
Goals:
- -Restore full knee ROM
- -Improve LE strength and endurance
- -Enhance proprioception, balance, and neuromuscular control
Precautions:
- -No Agility or plyometrics as these but significant stress on a maturing graft
Exercises/Treatment (Day 22 through 35)
- -Continue all relevant previous treatment and progress resistance as tolerated
- -Leg press (0-600)
- -Knee extension (90-400)
- -Progress hip and core musculature strengthening
- -Forward Step-ups
- -Lateral Step-ups
- -Lateral mini band walks
- -Initiate pool program when incisions are fully healed
- -Initiate dynamic stretching
- -Retro-walking on treadmill
- -Pool running
- -Reverse lunges
- -Progress to multi-directional lunging
ADVANCED STRENGTHENING AND PROPRIOCEPTION PHASE (3 months to 7.5 months)
- -Criteria for Phase Progression:
- -No pain or joint effusion
- -Full ROM
- -Quad strength 5/5 or higher
- -Subjective / functional knee scoring to 80% or higher
Goals:
- -Normalize LE strength
- -Enhance muscular power and endurance
- -Improve neuromuscular control
- -Restore Normal Functional Movement Patterns
- -Perform selected foundational sport-specific drills without cutting/pivoting.
- -Initiate interval walk/run program if able to meet pre-determined criteria
Exercises/Treatment (Weeks 14-16)
- -Continue all relevant, previous treatment
Tests- Isokinetic Test 10-12 weeks and 16-18 weeks
RETURN TO ACTIVITY PHASE (Months 7.5- 9months)
Criteria for Phase Progression:
- -Interval running
- -Quadriceps torque / body weight ratio (55% or greater)
- -Hamstrings / Quadriceps ratio (70% or greater)
- -Able to perform quality single leg squat to 450
- -Able to perform 70% maximum contralateral leg press
- -Able to perform brisk walk for 20 minutes
- -Able to perform reciprocal bounding for 50 feet with good form
Goals:
- -Achieve maximal strength and endurance
- -Progress skill training
- -Progress proprioception / balance skills
- -Progress power
Exercises/Treatment:
- -Continue all relevant exercises / treatment
- -Progress overall strengthening / plyometric exercise
- -Progress sport specific drills
DISCHARGE TESTING 1 PLANNING (typically done 9-12 months)
- -Based on a patient’s age, gender, and level that they are returning to (i.e. recreational, amateur, professional) a decision is made to endorse their return to sport/ higher level activity or to ask the patient to refrain from doing so. Currently our criterion includes, but is not always limited to the following.
-Symmetrical and acceptable comprehensive scores on CKC LE testing
-At least 90% symmetry when comparing right to left side per isokinetic test for the hamstrings and quadriceps
- -Not all patients who have undergone ACL reconstruction are candidates for functional testing. Those undergoing these tests should be chosen with proper consideration given to what they plan to return to and their general fitness level.
- -Patients often schedule periodically during this phase to assess their progress and properly change their program until they are deemed safe to return to all activities.
Updated 16JAN22:
Adam Anz, MD
Tyler Opitz, DPT, SCS, CSCS
Michael Polascik, ATC
References:
Charles D, White R, Reyes C, Palmer D. Effects of Blood Flow Restriction Training on Clinical Outcomes for Patients with ACL Reconstruction: A Systematic Review. Int J Sports Phys Ther. 2020 Dec;15(6):882-891.
Tucker A, Maass A, Bain D, Chen LH, Azzam M, Dawson H, et al. Augmentation of venous, arterial and microvascular blood supply in the leg by isometric neuromuscular stimulation via the peroneal nerve. The International journal of angiology: official publication of the International College of Angiology, Inc. 2010 Spring; 19(1):e31-7.
For additional information on revision ACL reconstruction surgery, or to learn more about common knee injuries involving one or more ligaments within the knee, please contact the Gulf Breeze, Florida orthopedic surgeon, Dr. Adam Anz located at the Andrews Institute.
Sources:




