Articular Cartilage Defect Surgery
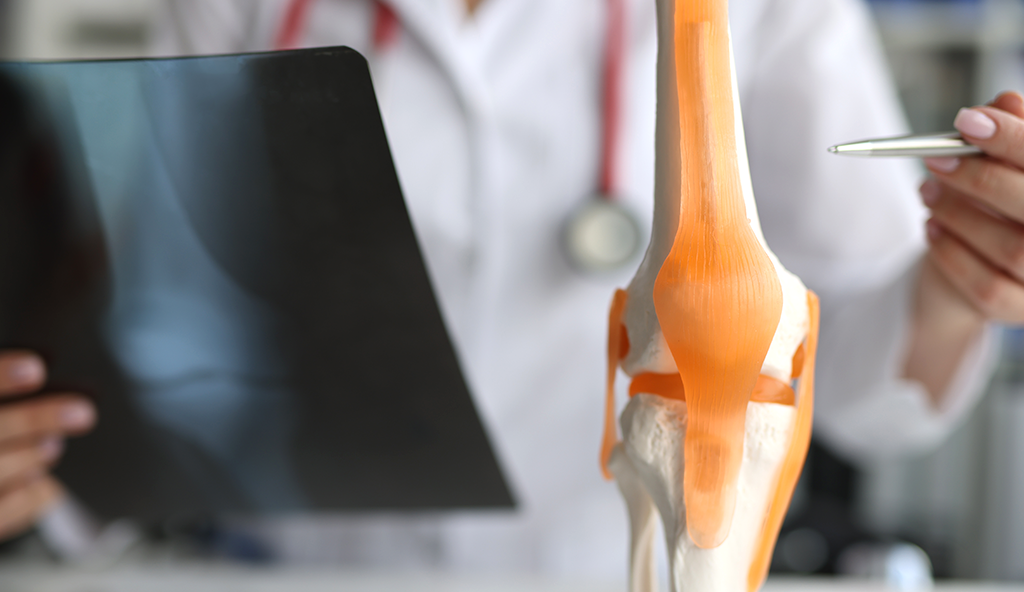
Articular cartilage is a very important component of a healthy knee joint. It covers the ends of each of the bones and is what allows for a fluid, smooth, painless motion of the knee. When an area of the cartilage becomes damaged, a patient will experience swelling and pain with activities, and over time, this process will continue to progress which eventually leads to complete loss of cartilage down to the bone. When this happens, a diseases known as osteoarthritis becomes present. This continues to cause progressive symptoms of knee pain and stiffness.
When a patient presents with damage to the articular cartilage, or an articular cartilage defect, it is of the utmost importance to treat this appropriately in an effort to restore the damaged area and preserve the surrounding cartilage. This treatment will depend on many factors including size of the defect, depth, location, associated injuries in the knee, age, and activity goals. In many cases with a focal cartilage defect, surgery is recommended.
There are a variety of surgical procedures that can be used to treat articular cartilage damage. These include chondroplasty, Microfracture, osteochaondral autograft transfer, or osteonchondral allograft transplantation. Listed below are some of the specific behind each technique:
- Chrondoplasty is an arthroscopic procedure used on some patients which involves using a camera and small instruments to trim away the damaged area of cartilage to alleviate the patient’s symptoms and prevent further propagation of the defect. This procedure is typically undertaken in patients who do not have full thickness defects (down to bone).
- Microfracture is a technique used in patients who have a full thickens loss of cartilage. It is a technique where a small pick is used to make holes in the bony surface of the defect. This allows the flow of marrow elements and stem cells which form a clot over the defect and eventually cover the area with a fibrocartilage layer.
- Osteochondral autograft transfer and osteonchondral allograft transplantations are two types of procedures where an autograft (taken from the patient) or allograft (taken from a donor) is used. In autograft OATs, small plugs of cartilage and bone are taken from another less important area of the patient’s knee and transferred in to fill the defect. In allograft OATs, the cartilage and bone are taken from a donor and also used to fill the defect. These procedures are done with a combination of arthroscopic and open techniques.
Physical therapy will be prescribed following surgery for an articular cartilage defect. Post-operative management varies depending on the specific type of procedure and the severity of the injury. For chondroplasty, patients are typically on crutches for a few days and allowed to weight bear as tolerated with full range of motion. For the other procedures the patient is placed into a brace and weight bearing is protected for 6-8 weeks. Motion may be initially restricted and a continuous passive motion machine (CPM) is also typically used for 6 weeks after surgery.
For additional information on osteoarthritis of the knee, or to schedule an appointment to discuss articular cartilage defect surgery or other treatments for this specific condition, please contact the Gulf Breeze, Florida orthopedic surgeon, Dr. Adam Anz located at the Andrews Institute.