The menisci are c-shaped, rubber-like cartilage discs that reside inside the knee joint. There are two menisci in every knee, one on the inner side (medial meniscus) and one on the outer side (lateral meniscus). Their function is to increase surface area for weight transmission between the cartilage on the ends of the bone, which decreases pressure between the ends of the bone and adds to stability of the joint. Both the medial and lateral menisci have stout attachments at the front and back of the tibia, these attachments are often called “roots”. These meniscal roots are important because they hold the meniscus in place to provide stability to the entire meniscus. The stability is obtained by a functional circumferential hoop which the C-shape obtains with attaching at the roots. This functional hoop stability prevents the meniscus from extruding out when pressure is exerted across the joint, effectively keeping the meniscus in place between the two bones.
Meniscus tears can occur in a number of different shapes and scenarios. They can occur as a result of accumulative wear and tear of the joint or as the result of an injury. Sometimes, wear and tear changes in the meniscus can be subtle until an injury event occurs and the scenario is worsened drastically. Tears of the meniscus root are especially concerning because they compromise the functional hoop property of the meniscus, rendering the meniscus non-functional. When there is a tear of the meniscal root the studies have suggested that pressure upon the cartilage is increased to levels similar to having no meniscus at all. This can subsequently cause early degeneration of the joint.
Meniscus root tears are often seen in two groups of patients:
- The first group consists of young adults and athletes who sustain a root tear with a severe knee injury. This may include injury to the ACL, PCL or other ligaments of the knee. Failure to repair the meniscal root in these circumstances can lead to the development of early osteoarthritis, failure of a ligament reconstruction graft and other potential problems with age.
- The second group of patients are middle-aged adults. In this population, the injury is “acute on chronic”. There are degenerative changes at the root and then the meniscal root becomes non-functional with an injury event. A sudden knee bending event accompanied by a “pop” in the back of the knee, is often described by patients who have had a root tear. A sudden deep squat or twist are also sometimes described. In this group of patients, rapid development of osteoarthritis can occur.
Symptoms
The primary symptoms of a meniscus root tear include pain on the inside or outside of the knee with mechanical symptoms. Certain activities such as pivoting, running, climbing, or even getting up from a chair may produce symptoms including popping and catching. Patients may hear or feel a clicking sound with movement, and the knee may be tender to the touch for some in specific locations.
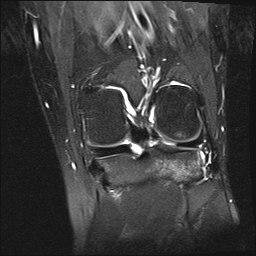
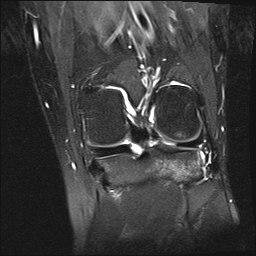
Figure 1, Coronal view of normal meniscal root
Diagnosis
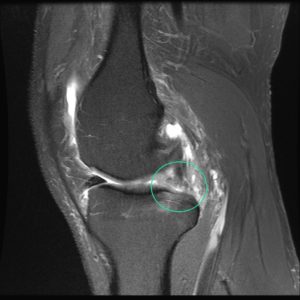
While an X-ray will not show meniscal damage, it is necessary to evaluate the overall health of the knee joint, as subtle changes on X-rays are common and help to guide treatment. Although a history, physical exam and x-ray are important in diagnosis, an MRI is important to visualize the meniscal root (Figure 1). These root tears can be very difficult to identify on MRI but is most often diagnosed when a “ghost sign” is seen. Meniscal root tears can be seen on coronal, axial and sagittal MRI views. On the sagittal view, as seen in figure 3, there is a ghost sign which is indicative of a meniscal root tear. A normal, healthy meniscus should look like a dark black triangle. On the coronal view, as seen in figure 2, there is a tear of the meniscal root.

Figure 2, Coronal View with “Ghost Sign”
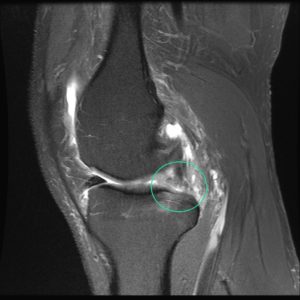
Figure 3, Sagittal View with “Ghost Sign”
Surgical Treatment
Treatment of meniscal root tears can be very difficult, especially in older patients. In older patients, repair can be difficult as tears are not commonly diagnosed until progression of arthritis is more severe. In younger patients, repair is much easier due to decreased prevalence of joint degeneration.

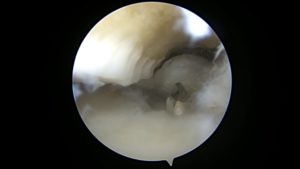
Figure 4, Normal Meniscal Root
An arthroscopic approach is utilized to repair the meniscal root. Once access is made into the knee, Dr. Anz will visualize the meniscal root (Figure 4). A device is used to pull on the root to confirm the presence of a tear. After a tear is confirmed, Dr. Anz will use a guide to drill a tunnel at the anatomic site of the original root. (Figure 5) This tunnel will become the new home for the torn meniscal root. Sutures will be passed through the torn portion (Figure 6) of the meniscus and shuttled down into the tunnel previously drilled. Once the sutures have been pulled into the tunnel, Dr. Anz will visualize the meniscus and tighten the sutures and secure them with a suture anchor.
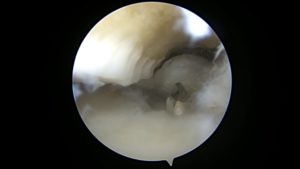
Figure 5, Drill bit coming up from root attachment

Figure 6, Sutures passed through the root repair
Post-Operative
After surgery, the patient will be non-weight bearing for 6 weeks to allow for healing of the repair. Physical therapy may be initiated the day after surgery. Range of motion at the knee is limited to 90 degrees of flexion for the first weeks in order to prevent excess stress on the repair. Six weeks after surgery a partial protective weight bearing program is initiated to slowly wean from the crutches. Patients should avoid impact activities, deep squats, and lifting in a deep squat for a minimum of 4 months after surgery to protect the meniscus root repair.
For more information on meniscus injuries, or to learn more about the surgical treatments for meniscus tears offered by Dr. Adam Anz, Orthopedic Surgeon/Sports Medicine Specialist, please contact our office.
[social_warfare buttons=”facebook,twitter”]