Injury Overview
Rotator cuff injuries are a very common cause of shoulder dysfunction in both young and old patients. The rotator cuff is comprised of a group of four muscle-tendon units that surround the shoulder joint and allow for overhead motion of the arm. The muscles and tendons that make up the rotator cuff also help stabilize the shoulder joint. A rotator cuff injury can occur when any of these muscle-tendon units become damaged. This is typically characterized by a separation or “tearing” of the tendon attachment off of the humerus. This can occur due to a number of factors, including:
- Acute injury – Such as a hard hit or traumatic fall sustained in a sport or car accident
- Chronic overuse – Continuous, repetitive movement that occurs with athletic training in activities such as baseball (pitching) or performing overhead movements like in tennis or swimming. On the job lifting of heavy objects can also lead to overuse.
- Gradual aging – the degeneration of the muscles or tendons over time and normal wear and tear can cause a breakdown of collagen, thus making the tendons and muscles more prone to degeneration and injury.
When any of these risk factors are present, the rotator cuff may be at risk for a tear. Certain other conditions, such as impingement and tendonitis, can also contribute to tearing of the rotator cuff. These tears result in a significant amount of shoulder pain, weakness, and limited range of motion. The severity of the injury may range from a mild strain with associated inflammation to a partial or complete tear that might require surgery.
Symptoms
The symptoms of a rotator cuff injury arise from the inflammation that accompanies the structural damage. The most common symptom is pain over the top of the shoulder and arm. In some patients, the pain can descend down the arm towards the elbow. This pain is evident at rest and may interfere with sleep at night, especially when lying on the affected shoulder.
Another common symptom typically associated with a rotator cuff injury includes weakness of the shoulder in combination with pain, causing difficulty in lifting the arm up in overhead motions or performing seemingly simple tasks such as getting dressed or reaching up to grasp an object.
Diagnostic Testing
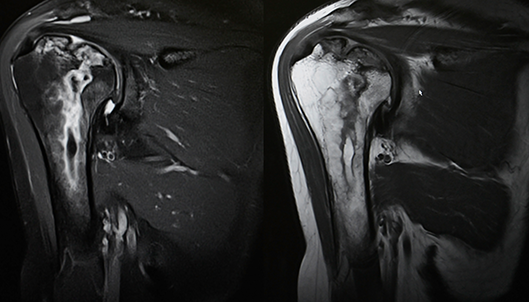
Dr. Anz will conduct a thorough examination and will observe the shoulder joint to look for deformities, muscle wasting, or weakness of the affected rotator cuff muscles. He will touch and manipulate the bones and muscles that make up the shoulder joint to find areas of tenderness or pain. He will carefully check overall mobility and strength. In addition, a variety of tests may be utilized to determine which of the muscles or tendons of the rotator cuff is damaged including X-rays (to look at the joint) or an MRI (to assess the soft tissue and cartilage).
Treatment
Most rotator cuff injuries can initially be treated without surgery. The success of non-surgical treatment options depends on the type of rotator cuff injury (acute versus more established), the size of the tear as determined by the diagnostic tests, and the activities of the patient.
Non-surgical
The goal of treatment is to reduce inflammation and strengthen the uninjured muscles around the shoulder to compensate for the torn or injured muscles or tendons. Some conditions may be easily treated with a combination of ice and heat, rest and diminished use of the shoulder for a determined amount of time. Anti-inflammatory medications (NSAIDs) can also help.
Some patients may require the assistance of a physical therapist to help strengthen the muscle and increase flexibility through a special exercise program. Dr. Anz may inject a steroid, such as cortisone, into the area of inflammation if the pain persists. The cortisone shot is designed to act only in the area where it is injected and has a potent anti-inflammatory effect.
Surgical
The need to surgically repair a rotator cuff injury depends upon your age, activity level, and the severity of your injury. Dr. Anz strives to achieve maximum recovery with minimal surgery and often prefers an arthroscopic treatment approach:
Arthroscopic Rotator Cuff Repair
An arthroscopic rotator cuff repair is done through a series of small incisions. Dr. Anz utilizes a small camera to view the damaged tissue on a large television screen. He is then able to insert small instruments into the joint to achieve the repair. The advantage of arthroscopic surgery is that there is usually less pain and a faster return to normal activities.
Post-Op
A rehabilitation program will be prescribed at your first post-operative visit with Dr. Anz. This will usually entail a period of rest and minimal rehab to allow the repair to heal. After healing is achieved, a more aggressive regimen is prescribed with the goal of regaining motion and strength.
Rehabilitation after surgery is as important as the surgical repair itself. Without proper rehab, the chance of full recovery is diminished. Patients are advised to be good to the shoulder as the rotator cuff heals by avoiding extra and unnecessary physical stress.
—
For more information on rotator cuff injuries, or for additional resources on shoulder injuries, please contact the Gulf Breeze, Florida orthopedic surgeon, Dr. Adam Anz located at the Andrews Institute.