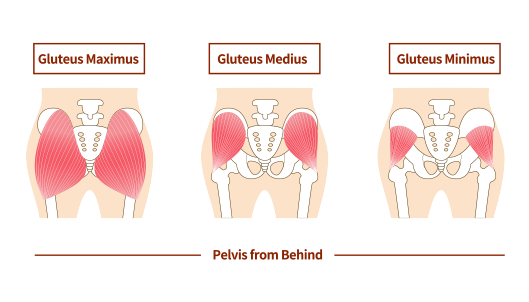
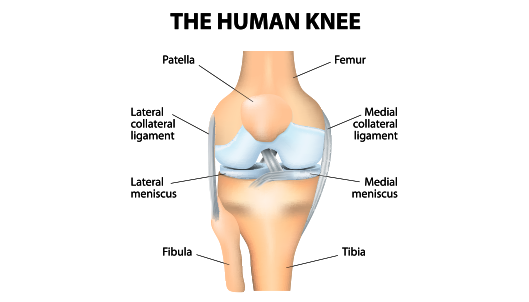
The iliopsoas (Psoas) is a muscle that originates within the pelvis and passes over the front of the hip joint before inserting on the femur (thighbone) at the lesser trochanter. As it travels from inside the pelvis to the femur it starts as a muscle and transitions to a tendon. The primary function of the iliopsoas is to flex the hip joint (serve to bring the knee to the chest). In some instances this tendon/muscle can become irritated and/or tight. Athletes and individuals who engage in sports or activities (such as running and sprinting) that involve rapid and repetitive hip flexion are at a greater risk for injury of this muscle/tendon. If the iliopsoas is tight for a long period, it may rub across the front of the hip joint and cause a snapping sensation and/or damage to structures of the hip, a scenario known as psoas impingement. Psoas impingment can be accompanied by significant pain and disability and when accompanied by a snapping sensation and/or sound is referred to as “internal snapping hip syndrome.”
Dr. Anz will evaluate a patients symptoms and physical examination. The first step for treating psoas impingement is a trial of stretching, anti-inflammatories, physical therapy, and rest. In many cases, the inflammation will resolve and the symptoms decrease. A trial of physical therapy is necessary with a goal of guided stretching and hip strengthening.
If pain and snapping sensations do not improve, Dr. Anz may recommend surgery to lengthen the muscle/tendon unit. The iliopsoas is an important stabilizer of the hip joint, so for some patients this may not be the best option. Dr. Anz will determine if this approach will offer the best outcome based on a patient-by-patient basis. When a psoas lengthening is deemed appropriate, he will use an arthroscopic approach. During surgery, keyhole incisions are used at the hip where he can insert a small camera and surgical tools to view the inside of the hip joint and perform the lengthening. To relieve tightness and eliminate the symptoms of the tendon rubbing over the front of the pelvis, Dr. Anz will release the tendon portion of the iliopsoas at the hip leaving the muscle portion of the iliopsoas intact. This lengthening leaves the hip flexor attached to the femur, but releases the tension creating the problem.
Following arthroscopic hip surgery for psoas hip impingement, Dr. Anz will prescribe a through rehabilitation program. This will consist of a progressive plan that will involve week-by-week rehabilitation exercises and a set of recommended protocols. Depending on the length of prior symptoms and associated injury, most patients are able to return to their previous activities within 4-6 months following surgery.
For additional information on the treatment for psoas impingement, or to learn more about arthroscopic hip surgery and partial psoas lengthening, please contact the Gulf Breeze, Florida orthopedic surgeon, Dr. Adam Anz located at the Andrews Institute.