Multi-ligament knee injuries are serious injuries that are often considered complex. This type of injury occurs when more than one ligament is affected during injury. There are four major ligaments that make up the knee joint. Each has their own function but together they work to stabilize the knee.
These ligaments include:
- The anterior cruciate ligament (ACL)
- The posterior cruciate ligament (PCL)
- The Medial collateral ligament (MCL)
- The Posterior lateral complex (PLC)
Multi-ligament knee injuries can occur as the result of a traumatic incident such as a collision or fall during sports, an automobile accident, or a serious fall such as snow skiing. Each injury is different and depending on different mechanisms, a multitude of injury patterns can be present.
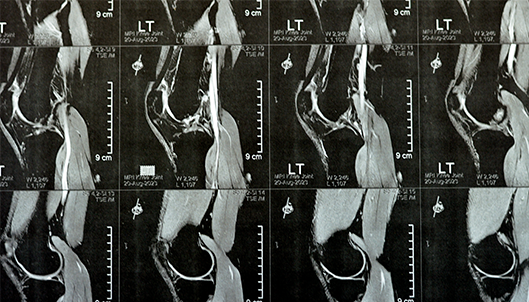
In many instances where multiple ligaments are affected, a multi-ligament knee reconstruction would most likely need to take place. An MRI will be able to detail the extent of the ligament injury. When multiple ligaments are involved, there are occasions where one ligament can heal on its own while another is reconstructed, and there are occasions where more than one, or multiple, ligaments must be reconstructed.

Reconstruction of ligaments such as the ACL and PCL requires removing the damaged ligament and reconstructing a new ligament with a graft. This graft may be from the patient’s own tissue (known as an autograft), or it could be from donated tissue from another person (known as an allograft). In some instances, it may be necessary to use multiple allografts. The goal of this surgery is to attempt to secure the ligaments back to their native position. Dr. Anz will often perform this surgery in one operation and once the ligaments are attached back to their anatomic sites, during early post-op, one can start early range of motion to minimize the chance of the patient developing stiffness and scaring around the knee.
Following this surgical procedure, physical therapy will begin immediately; however, knee range of motion may be limited for a period of time. Bracing and progression with therapy is individualized based upon the type of injury. Multi-ligament knee surgeries are serious procedures and a thorough, and intensive rehabilitation program will need to be followed post-op in order to obtain the most optimal results.
—
For additional information on multi-ligament knee injuries, or to learn more about multi-ligament knee reconstruction, please contact the Gulf Breeze, Florida orthopedic surgeon, Dr. Adam Anz located at the Andrews Institute.