Arthritis of the shoulder is a common, degenerative condition that affects the adult population.
Sometimes brought on from a previous shoulder injury, and other times developing due to the aging process and natural wear and tear of the shoulder joint, arthritis can cause pain, stiffness, and shoulder weakness that makes normal daily activities difficult to perform.
Once all conservative treatment measures—both non-surgical and surgical—have been explored and/or tried, replacement surgery can be the next step in helping to alleviate some of the symptoms that occur with arthritis of the shoulder.
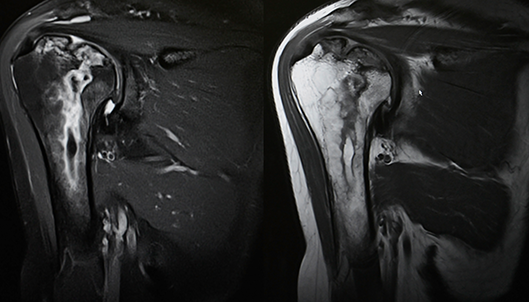
A reverse shoulder replacement surgery, like a standard shoulder replacement, involves replacing the natural degenerated cartilage and bone of the shoulder joint with metal and plastic components. These components allow patients to have a more mobile, painless, motion of the shoulder joint. The reverse total shoulder replacement technique is not for everyone. In patients who have rotator cuff surgery/arthropathy, the rotator cuff muscles may no longer function as they should, therefore, the reverse total shoulder replacement surgery is a better fit because it relies on different muscles (the deltoids) in order to create shoulder movement. A traditional replacement approach relies on the rotator cuff muscles to function.
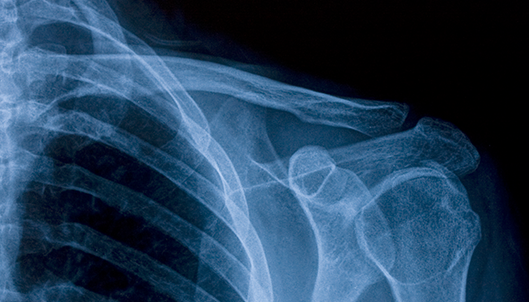
The surgical approach for a reverse total shoulder replacement is similar in nature to the total shoulder replacement surgery. In a standard shoulder replacement, the head of the humerus is replaced with a rounded metal component attached to a stem that is fitted into the humerus. Additionally, the glenoid portion of the shoulder blade, or socket of the shoulder joint, is replaced with a plastic socket. In a reverse shoulder replacement, the shape positions are reversed, so that the glenoid becomes a rounded partial sphere and the arm portion, humeral component, involves the socket.
Patients who have experienced rotator cuff problems and who have undergone reverse total shoulder replacement surgery have experienced good result in eliminating their shoulder pain, and regaining mobility and function.
After shoulder replacement surgery, patients are placed into a rehabilitation program. It is important for patients to follow rehab closely as this therapeutic process is as important as the surgery itself in reaching a full recovery. Initial therapy focuses on safe motion with certain restrictions for 6 weeks. After a recovery period of 2-3 months, patients typically are painless and performing well with their normal activities. A return to sporting activities is patient and activity dependent.
—
For additional resources on treatment for shoulder pain and stiffness for injuries associated with osteoarthritis of the shoulder, or to learn more about the reverse total shoulder replacement surgery, please contact the Gulf Breeze, Florida orthopedic surgeon, Dr. Adam Anz located at the Andrews Institute.